Despite significant advancements in technology adoption in healthcare, many providers in the sector are having difficulty embracing and realising the full potential of healthcare technologies (healthtech).
TeleHealth, which is shorthand for providing health-related services through telecommunication technologies, underwent a rapid acceleration of adoption when the COVID-19 pandemic began. Since then, the majority of patients have embraced the convenience of digital engagement and virtual care options for enhanced access to personalised, high-quality care and follow-up monitoring.
However, at the same time, an alarming number of physicians and providers have scaled back their use of TeleHealth as they struggle to keep up with the increasing demand for virtual visits and health condition remote monitoring at scale, creating a shift in patient-physician relationships.
Here at Webhelp, we see the same issue across the entire spectrum of HealthTech — consumers are on-board, but providers are often slower on the technology adoption in healthcare. This trend extends to almost every technology offered within the consumer care and healthcare system, especially software and physical solutions that create new digital diagnosis or treatment opportunities.
We believe that adequate communication and related solutions are the key components to solving these challenges, so this article outlines several strategies for aligning patient and physician perspectives and empowering providers with the full potential of HealthTech solutions.
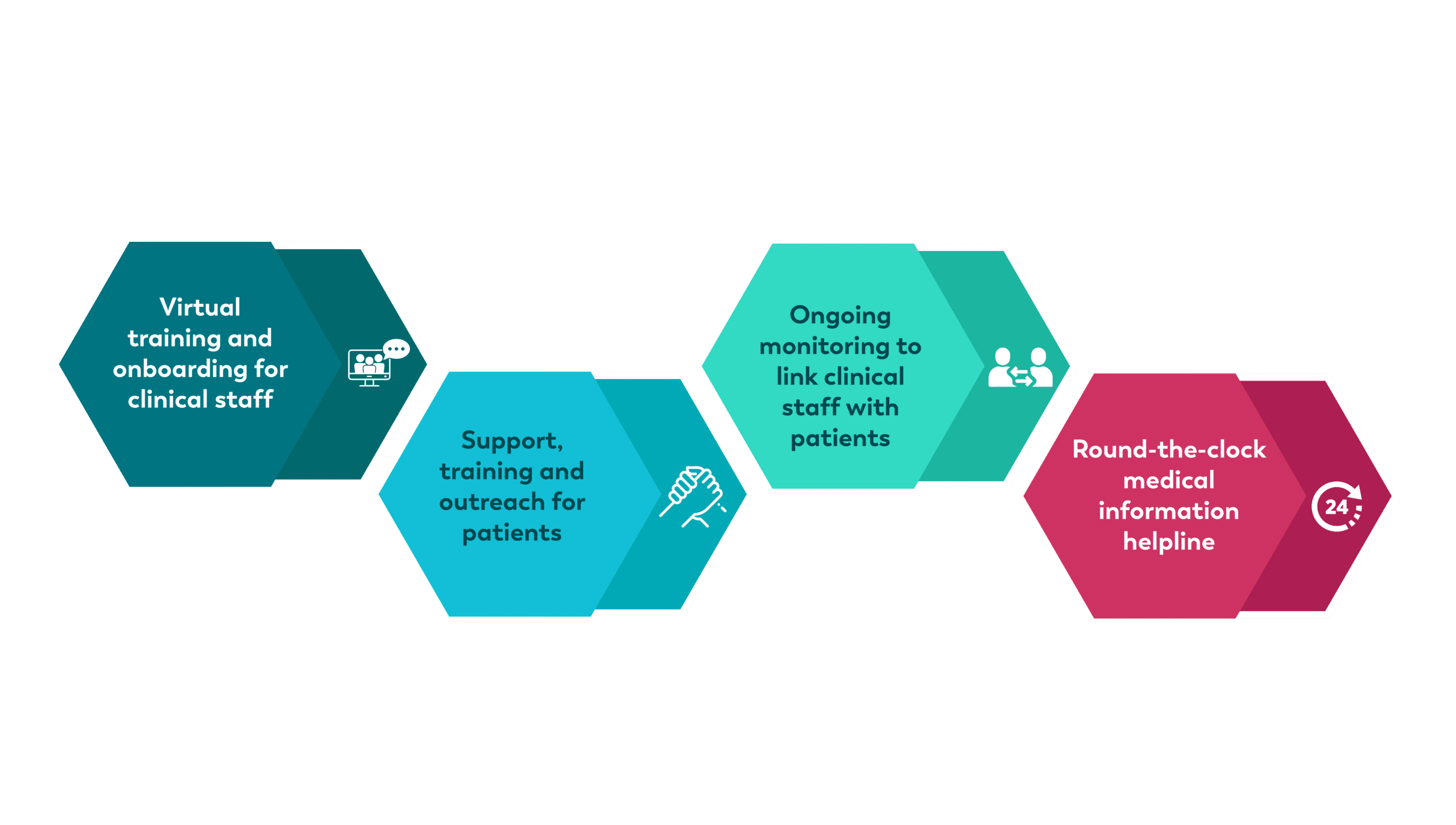
Technology Adoption in Healthcare
Virtual training and onboarding for clinical staff
A great starting point is to help healthcare professionals to understand the benefits that healthcare applications and similar HealthTech tools can provide.
During this process, representatives can inform, train, and onboard doctors at their offices, in the hospital or online. Additionally, this is an ideal opportunity to host webinars and introduce multidisciplinary boards into the process – a medical science liaison, for example.
By organising these virtual events through digital channels, providers can understand everyone’s preferences in-depth, monitor the information provided, analyse attendance trends and obtain valuable feedback to inform future strategic planning. As previously reported at Webhelp Medica, providers have begun offering webinars, remote workshop sessions, and social networks intended solely for clinical staff, suggesting that the industry is open to digitising its communication endeavours. Now it’s just a matter of increasing adoption.
Support, training and outreach for patients
As part of this solution, providers could run informative campaigns to build awareness of the different healthcare apps available whilst implementing patient support programs for specific treatments and drugs. Providing motivational calls to help patients understand the benefits of these is a proven enabler.
Once implemented, nurses can teach patients to be autonomous in their treatment, such as administering injections themselves at home. Once the patient becomes responsible for this process, the nurses can carry out continuous remote monitoring, including as part of virtual wards through SMS or other channels, enabling patients to follow treatment and monitoring plans independently in their own homes. When Webhelp Medica implemented a self-injection learning program for almost 3,000 patients, 99% of physicians and 93% of patients were highly satisfied with the approach, highlighting the efficacy of combining nurses with digital support.
These initiatives become game-changing for non-tech users and vulnerable or immobile patients, especially when coupled with the creation of online patient groups where people can discuss their pathology with others in the same situation. Equally, it’s crucial to include caregivers, families, spouses, and patient associations to expand these groups further and provide more support and autonomy for patients.
We like to think of this process as creating “expert patients” trained in their pathology with the knowledge to help other patients with their treatment routines, lessening the burden on clinical staff. It also allows physicians to strengthen their relationships with patients by enrolling them in coaching and learning programs.
Ongoing monitoring to link clinical staff with patients
Once engaging with clinical staff and patients through training, onboarding, and outreach, the monitoring and follow-up process is where the optimisation of patient-provider communication flourishes. By customising patient journeys based on their uptake of technology and putting digital technology at the heart of the follow-up wherever appropriate, clinical staff can vastly increase patient awareness of the importance of care continuity.
While it’s essential to determine whether patients feel comfortable talking with health professionals remotely, virtual monitoring ensures that problems and concerns can be solved quickly, efficiently, and effectively for many pathologies. For example, for psychological and behavioural follow-ups, providers can install a team of remote nurses and psychologists, or even tobacco specialists and dieticians, to follow the patient’s progress and provide guidance and advice via digital platforms or telephone calls.
For tech-savvy patients, there’s an opportunity to apply conversational SMS platforms and social messaging tools to communicate with clinical staff instantaneously. Clinical staff can also automate appointment and medication reminders to reduce the rate of no-shows and ensure patients stay on track with treatment plans. Plus, providing an inbound line allows autonomous patients to ask questions if they have any doubts about their treatment.
In another example, providers could email patients a QR code that refers to an informative video explaining, presenting, and informing people on their pathology, treatment follow-up, and tips for improved well-being. After a teleconsultation, physicians could also automate a message to check in on long-term patients and ask if they have questions about their treatment.
When implemented correctly, virtual wards and outpatient monitoring processes like these bring clinicians and patients closer together, preventing communication challenges before they occur.
Round-the-clock medical information helpline
Another relatively untapped communications solution is a readily available information helpline operating 24 hours a day, 7 days a week. An incoming medical information line can provide patients with status updates on product availability, medication request follow-ups, medical information requests, patient data and held information, pharmacist information, specific questions from a doctor, and pharmacovigilance.
With these four communications strategies and solutions, healthcare providers can improve their relationship with HealthTech, encouraging physicians to share the same enthusiasm for technological evolution as their patients.